A virus with a nearly 100% infection rate could increase the risk of developing Alzheimer’s disease.
The idea that Alzheimer’s disease may be caused in part by microbial infections has been around for decades and recently started to gain increased support with the scientific community. Hundreds of studies have observed an increased incidence of many types of infections in Alzheimer’s disease patients. However, most of these studies could not establish a direct causative link, and they provided little insight into the mechanisms of this interaction.
Recently, a study published in the journal Neuron provided some of the strongest evidence yet for the infectious theory of Alzheimer’s. Researches from the Icahn School of Medicine at Mount Sinai collected portmortem brain samples from people with preclinical Alzheimer’s disease, as well as healthy controls, and used an advanced laser-capture technology to analyze the gene expression in their neurons. They then constructed computational models to predict which patterns of gene expression were associated with Alzheimer’s disease. They noticed that many of these genes that had different expression in the Alzheimer’s brains played a role in immune system’s response to viral infection.
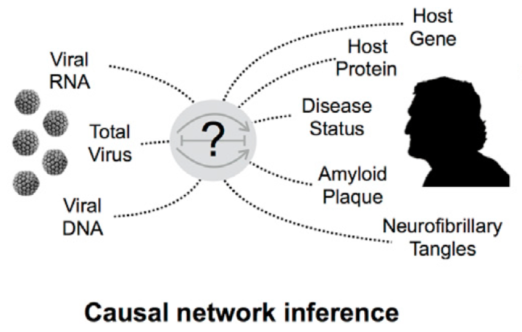
This figure from the paper illustrates how researchers employed computational models to connect viral infection rates with the signatures of Alzheimer’s disease.
To further investigate this viral connection, the researchers analyzed the levels of viral RNA in each of the brain samples. They found that the Alzheimer’s brains had significantly more RNA from two types of human herpes viruses (HHV): type 6A and type 7. (Note that HHV is not to be confused with human simplex virus [HSV], which is a sexually transmitted infection.) This suggests that people with Alzheimer’s disease have higher rates of HHV infection in their brains.
Furthermore, they found that the viral infections could perturb many genes that are linked to the development of Alzheimer’s disease, including BACE1, which helps create the sticky plaques that are characteristic of the Alzheimer’s brain. HHV-6A also decreases expression of a microRNA gene called miR-155. When they created mice that lacked expression of miR-155, these mice developed Alzheimer’s plaques in their brains, suggesting that this gene could be an important link between herpes infection and Alzheimer’s.
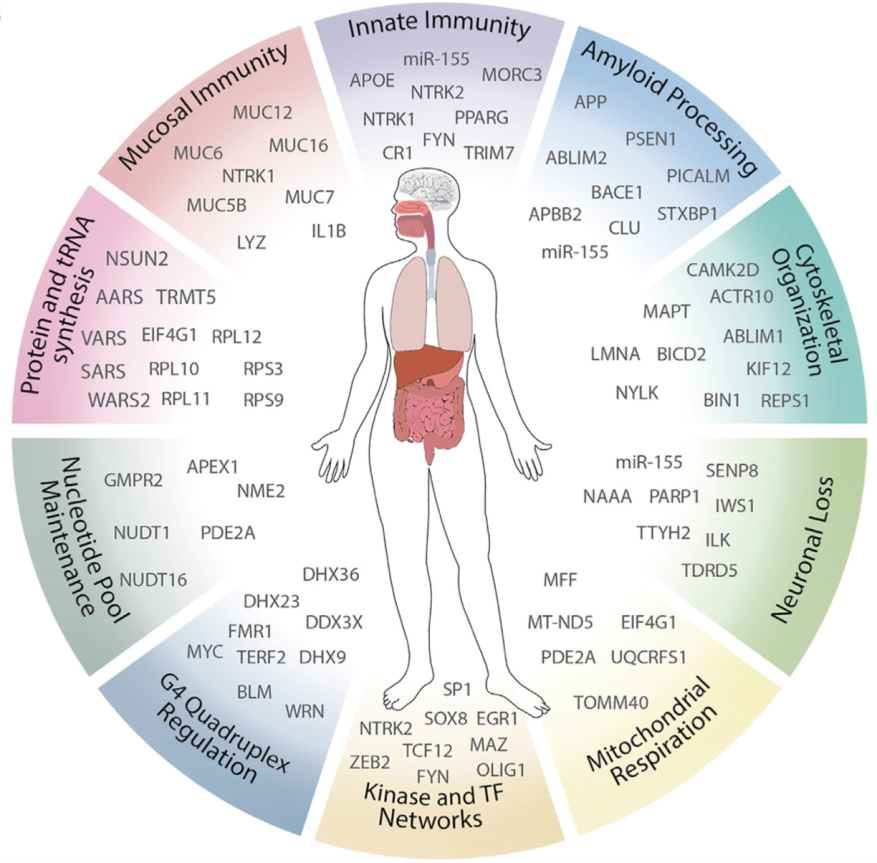
This figure from the paper shows the complex network of genes that may link herpes virus infection with the development of Alzheimer’s disease.
This study is different from previous ones in several ways. It includes a large sample size from throughout the United States, which provides higher statistical rigor to the conclusions. It also suggests a possible mechanisms by which viral infections could contribute to the development of Alzheimer’s disease via disruption of neuronal gene expression. The results support the intriguing possibility that the toxic amyloid-beta protein, which has long been thought to be the primary cause of Alzheimer’s disease, could actually be a beneficial response to viral infection, a theory that I described in a previous article. While this study is not yet conclusive proof that herpes infection can directly lead to Alzheimer’s disease, it opens that door for many interesting new avenues for research that should be investigated further.
A connection between herpes and Alzheimer’s disease is both troubling and encouraging. HHV types 6 and 7 are extremely common, with nearly 100% of individuals infected by age 3. Most of us are likely infected as infants through the saliva of our parents or other relatives. After the initial infection, the virus becomes latent and remains circulating in the bloodstream for life. For most of us, HHV-6 and HHV-7 infections are completely asymptomatic. However, as we grow older, our immune systems weaken, allowing these viruses to travel from the bloodstream to the brain. Some reports suggest that the resulting neuroinflammation could contribute to common age-related neurodegenerative disorders such as Alzheimer’s and Parkinson’s diseases.
Yet these results also offer hope. If microbial infections such as HHV are the initial cause of Alzheimer’s disease, this suggests that we could treat the disease using immunosuppressant or antiviral drugs. Should future studies confirm this to be true, this could be a huge boon for the development of effective Alzheimer’s therapies.