Unless you’ve been living under a rock for the past week, you’ve probably heard the big news: the FDA has just approved a new drug to treat Alzheimer’s disease, the first new treatment for this condition in nearly 20 years. At first glance, this should be exciting news. Alzheimer’s disease, a neurodegenerative memory loss disorder that affects 1 in 3 people over age 85, has been studied for more than a century with little apparent progress toward a cure. And now, Aducanumab (also called Aduhelm) has been approved! So… why aren’t scientists celebrating?
The Dream of a Cure for Alzheimer’s Disease
To explain the problems with Aducanumab, let’s first back up a bit. This is actually not the first drug that’s been approved by the FDA to treat Alzheimer’s disease. Other drugs like memantine have been on the market for decades. Memantine is designed to temporarily reduce the symptoms of Alzheimer’s disease by targeting NMDA receptors in the brain. Basically, since the neurons in your brain gradually die over the course of Alzheimer’s disease, memantine helps to boost the signaling power of your remaining neurons so that your symptoms are a bit less severe. However, it doesn’t prevent the neurons from dying, so eventually it stops being effective. As a result, memantine is only helpful for mild to moderate stages of Alzheimer’s disease, and it cannot slow the disease’s overall progression or improve the patient’s lifespan. Memantine is like taking a painkiller rather than treating the actual wound.
But Aducanumab is different. In contrast to previous drugs like memantine, Aducanumab is designed to treat the underlying cause of Alzheimer’s disease, not just its symptoms. The hope is that it could actually slow the disease’s progression, giving patients a few more months or even years of life before dementia sets in, or maybe even reversing their symptoms. If successful, this would be a true cure, not just a temporary band-aid.
Aducanumab, like the majority of drug candidates to treat Alzheimer’s disease, was designed based on the amyloid cascade hypothesis, which I’ve covered extensively in other articles. In simple terms, when you have Alzheimer’s disease, a toxic sticky protein called amyloid-beta gradually accumulates in your brain, becoming more widespread over time. The amyloid cascade hypothesis says that by reducing levels of amyloid-beta, we could slow or halt the disease’s progression.
And this makes sense: if you saw a patient whose brain was full of a toxic protein, you’d probably assume that getting rid of the protein would be the key to treating the disease. But after decades of research and hundreds of failed clinical trials, concrete evidence in favor of the amyloid cascade hypothesis has never materialized. Drugs have been invented that effectively reduce amyloid-beta in the brain, yet the patients showed minimal improvement in their symptoms, and some even got worse. Other studies have shown that many people can develop high levels of amyloid-beta in their brains without ever experiencing symptoms of Alzheimer’s disease.
After years of failed research, much of the neuroscientific community has moved on from the amyloid cascade hypothesis in favor of a more nuanced understanding of this disease. Maybe targeting another toxic protein called tau, which also accumulates in Alzheimer’s patients’ brains, will be more effective. Maybe amyloid-beta is an immune response and it’s actually brain infections that are to blame. Maybe accumulating metal ions are to blame. There are many new theories to explain the cause of Alzheimer’s disease, and it’s likely that all of them are correct to some degree, each contributing a small component of an individual’s overall risk for the disease. One thing, at least, seems clear: amyloid-beta alone is not enough to cause or to cure Alzheimer’s disease.
How Did We Get Here? The Story of Aducanumab
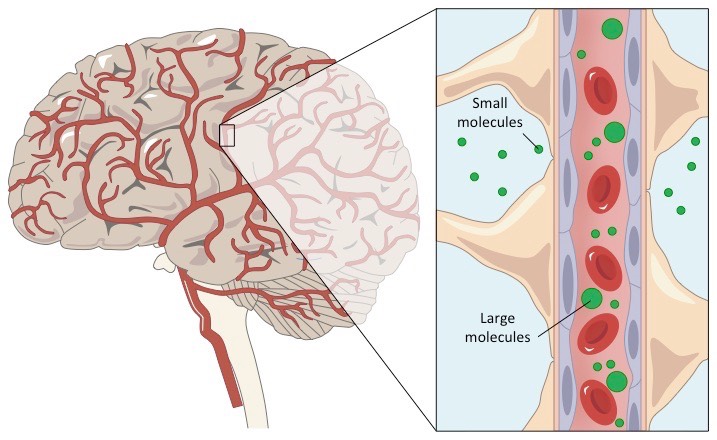
But let’s get back to Aducanumab. This drug is what’s called a monoclonal antibody. Essentially, it’s a small protein that’s designed to bind to amyloid-beta aggregates and help clear them out of the brain. To test this drug, Biogen (the company that makes Aducanumab) recruited nearly 2000 patients into two different phase 3 clinical trials, where they would receive either the drug or a placebo. After a three-month treatment period, the patients took a variety of cognitive tests to assess their dementia symptoms.
In March 2019, Biogen announced that they were suspending their Aducanumab clinical trials, stating that the drug did not show evidence of efficacy in treating the cognitive symptoms of Alzheimer’s disease. For a while, it seemed like that was that. Just another failed clinical trial for Alzheimer’s disease, as hundreds had failed before.
However, in October 2019, Biogen released another statement. They had repeated their analysis with an additional ~300 patients who were not included in the original calculations, and found that there was a detectable improvement in cognitive scores resulting from the treatment. That improvement was marginal, around 20%, though it did reach statistical significance. They applied for FDA approval through the accelerated pathway, which is the same pathway that was used to rapidly approve the COVID-19 vaccines. This pathway is designed to allow urgently-needed, potentially life-saving treatments to progress more quickly through the standard FDA approval pipeline, with the caveat that the companies must conduct additional studies in the future to confirm their efficacy.
The accelerated pathway made sense for the COVID-19 vaccines, which showed very high efficacy and mild side effects in clinical trials. In contrast, Aducanumab came with miniscule improvements in cognitive symptoms and a risk of severe side effects, including bleeding inside the brain, falling, and confusion/delirium. The drug did seem to be effective at reducing amyloid-beta levels, but as I explained above, this often does not correlate with any meaningful improvements for the patients. Perhaps unsurprisingly, when the FDA advisory committee reviewed the evidence in November 2020, they voted unanimously to reject Aducanumab for FDA approval.
While the advisory committee’s decisions are technically just a recommendation, the FDA almost always makes the final decision in line with their ruling. But in this case, the FDA went against the committee’s decision and approved Aducanumab via the accelerated pathway. This will allow Biogen to being selling the drug to patients almost immediately. They are required to conduct an additional trial with stronger evidence that the drug is effective, but these results are not due until 9 years from now, giving Biogen plenty of time to draw a profit in the meantime.
Though the FDA states that this decision was based on the evidence, it seems likely that external pressures played a role as well. The Alzheimer’s Association and the American Geriatrics Society both issued letters to the FDA urging them to approve the drug. Now, as someone who has been actively involved with the Alzheimer’s Association for years, I truly believe that both of these organizations acted in good faith. Alzheimer’s is such a devastating disease, and the past decades of failed research have been incredibly frustrating. I can understand why they would want to pursue that small glimmer of hope. But I’m concerned that the evidence is simply not on their side in this case.
The Enormous Costs of Aducanumab
Now you may be asking: so what? Maybe the drug isn’t that effective, maybe it’s not even effective at all. But what’s the harm? Shouldn’t we at least try it out and see if it helps people?
Even if we ignore the potential side effects, the financial implications of Aducanumab are set to be staggering. The drug is expected to cost each patient an average of $56,000 per year. Most of this cost will be shouldered by the taxpayers.
How much will this cost us? According to a recent article in The Atlantic, if we assume that only one-third of the six million Americans living with Alzheimer’s disease choose to take the drug, that adds up to $112 billion in annual healthcare spending. That’s more than Medicare spent on all prescription drugs combined during 2020! This drug has the potential to put extreme pressure on the Medicare and Medicaid systems, not to mention the remaining out-of-pocket costs that Alzheimer’s patients and their families will struggle to pay.
Now, if this drug were actually effective, I would argue that these financial costs would be well worth it, both for the improvements in patients’ quality of life and for the concrete fiscal benefits of reduced spending on long-term care facilities. But to take on such a financial burden for a drug whose benefit seems marginal at best… to be honest, I’m very worried. Furthermore, this drug sets a dangerous precedent for other pharmaceutical companies. What other drugs may be forced through the FDA approval pipeline based on shaky evidence and powerful lobbying?
Many other scientists and physicians have voiced their concern over Aducanumab. Dr. Jason Karlawish, a practicing physician and medical faculty at U Penn, wrote that he will not prescribe the drug to any of his patients. Dr. Robert Howard, a professor of old age psychiatry at University College London, stated, “Now, we’ll wait a decade before it becomes obvious to everyone that there are no benefits – only high healthcare costs –- associated with the treatment.” Even Dr. Derek Lowe, a well-known drug discovery researcher in the pharmaceutical industry, has cast his vote against the drug.
Conclusion: Where Do We Go From Here?
With all that said, here we are. Aducanumab is approved, and patients will start receiving the drug soon. Biogen has nearly a decade before they have to prove the treatment is really effective. Only time can tell how this will impact our healthcare system. I am worried that the FDA has gone over the heads of its own advisory committee, in the face of strong evidence against the amyloid cascade hypothesis, and made a decision that will have huge health and financial implications for years to come.
It’s a gloomy picture I’m painting here, but while I don’t personally have much faith in Aducanumab, I haven’t given up on the dream of curing Alzheimer’s disease. There are still many promising new avenues to explore for treating this condition and understanding its true cause. Broadly speaking, I’m optimistic about the future, and I hope that the implications of Aducanumab will not set us back too far.
Before I wrap this up, I want to make one thing clear to those of you who are living with Alzheimer’s or are close with someone who is. I am not saying that you, as an individual, should not take this drug. I’m also not saying that you should take it. That is a decision between you and your physician. Maybe this drug will turn out to be amazing, or maybe it will be a flop. In the meantime, we need to all make the best decisions we can based on the available evidence and our personal values.